The first time I ever felt I wanted to be a nurse, I was married with a 2-year-old daughter, Gianna, and a 6-week-old son, Dylan. I attended a nursing school information session at Northern Essex Community College (NECC) in 2005. Unfortunately, I allowed comments about how hard nursing school would be with two young kids to keep me from pursuing a career change.
Fast forward three years later to when I was a single mom raising my kids. My world was turned upside down when my father was diagnosed with a glioblastoma at the age of 59. It was his ICU nurse who made me want to pursue my dream, no matter the obstacles. I enrolled in classes at NECC to start my prerequisites while working, raising my kids and being one of my dad’s caretakers. I achieved this goal with the help of many others.
My father spent almost three weeks at High Pointe House in Haverhill, a home-like alternative to hospitalization with specialized end-of-life care. I was impressed and beyond grateful for the care he received from the nurses and care partners. I knew this was where I wanted to work.
My dad’s room was always filled with family and friends. Yes, we were that loud room. People were just drawn to my father. He had that energy about him his entire life.
While visiting my dad every day during those weeks, I remember other rooms with patients who never had visitors. It was that reason why I became a volunteer. Once I started the nursing program at Lawrence Memorial/Regis College, I volunteered at High Pointe House. I knew I had something to give back to patients and families. Part of what I was giving back was a true understanding of what they were going through.
I volunteered at High Pointe House for four years, until I graduated from nursing school in 2018. I sat with patients, read to them or wrote messages on a board if they got a phone call, but had a hard time hearing the voice on the other end. Sometimes patients ask to play a card game, or they just want company while they watch TV. Volunteers play an important role at High Pointe House, and we are missing them due to the COVID-19 crisis.
Never did I think I would encounter a pandemic during my nursing career, but here it is. Knowing I would be provided the proper personal protective equipment (PPE), I had no hesitations about working in the new precaution unit at High Pointe House. I’m proud to work at the first hospice house in Massachusetts that is caring for individuals at end of life who are also positive for COVID-19.
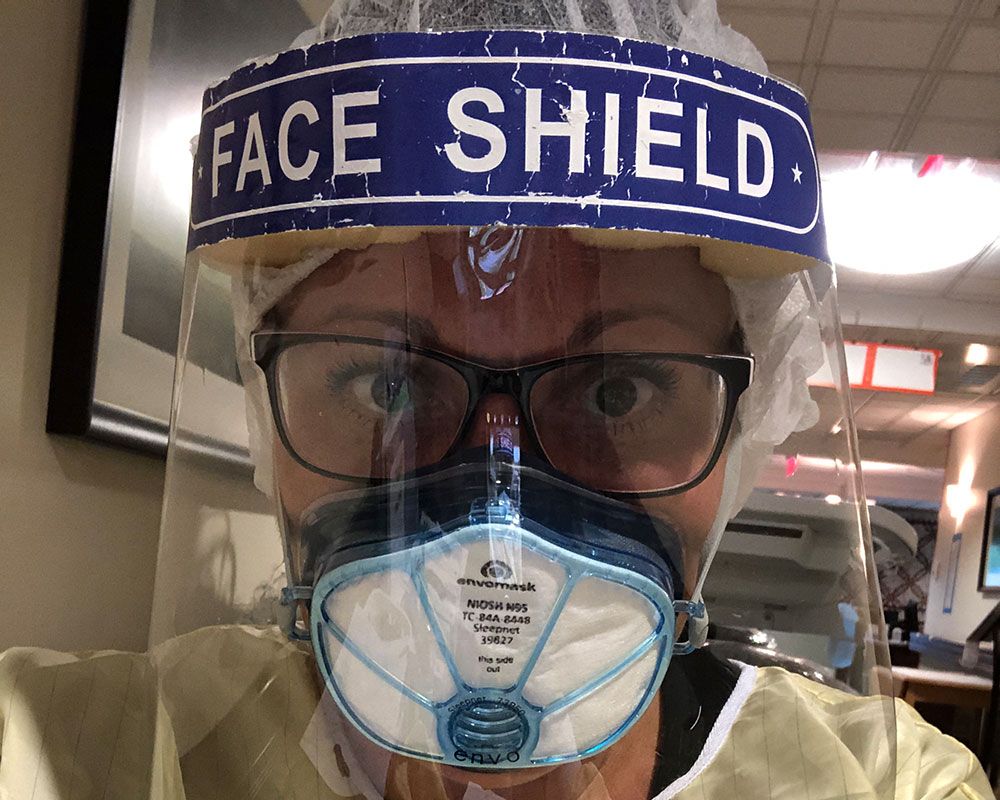
I arrive for my shift early because the nurse I’m replacing has been in PPE for hours, and I know how anxious I feel when it is getting close to the end of my shift. Prior to COVID, I enjoyed doing my hair and makeup for work. I was a hairstylist for 23 years before becoming a nurse, and I don’t think that love of doing hair and makeup ever goes away. But now my hair is always up and I don’t put on makeup. Instead, I wear a gown, Envo mask, face shield, two pairs of gloves and a hairnet.
During my shift, I work with a care partner. We are continuously checking our patients, giving scheduled medications as well as medications as needed to manage symptoms, and coordinating Skype calls with the nurse practitioner, social worker and chaplain. The hardest part is making phone calls with families to say goodbyes to their loved ones.
In between, documentation has to be done. That can be a challenge if you wear glasses because they always fog up. I am not one to sugarcoat anything, and there are a lot of moments when I feel very anxious in the mask. We have learned to go into an empty suite, open a window and get some fresh air.
I find I’m always talking to myself, saying it will be OK, but it’s tough. Patients can’t see a comforting smile when we walk into a room, and that is hard. Even more so when you can tell they are afraid and you want them to know it will be OK.
Patients with COVID-19 can have symptoms that need to be managed often. We do a lot of education with families. We want them to understand what we are doing for their loved ones, how we are treating their symptoms and assure them that they are comfortable.
Under the current guidelines, families are allowed to visit for an hour if their loved one’s passing is imminent. This is another difficult part. We are so used to patients being able to have their loved ones at the bedside when they pass. They have us nurses and care partners, but it’s not the same.
I am someone who doesn’t usually cry, but lately I have been crying a lot more. This is harder than we thought, and unless you work in this COVID unit, you will never understand the enormous impact this has on us. I’d give anything to go back to how it was. There is definitely a new respect for nurses, for which I am grateful.
At the end of my shift, when I finally get to take off my PPE, there is not a better feeling! I get dressed into a change of clothes, and everything is bleached and put into a bag. Once home, I shower and wash my scrubs right away.
Another tough part of this is coming home and having my son wait up for me. He waits up every time I work. He just wants to make sure I am OK. He knows at this point he can’t give me a hug or kiss. He has to wait until I am showered first. A positive note is my daughter, who really did not know what she wanted to do for a career, now knows she wants to be a nurse. I think that’s amazing.
I do feel safe in my PPE, and there’s no question I want to care for patients with COVID-19, just like any other communicable disease. Nurses have an amazing ability to hide their fear or anxiety and give all they have to deliver the best care for their patients. As hard as this is, I’m honored to be doing my part for my patients and community.
Although many news outlets take sides, WHAV does not. Views and comments expressed are those of the writer and are not intended to reflect the views of Public Media of New England Inc. d/b/a WHAV, its staff, underwriters or affiliates. Letters are published on a space and time availability basis and may be edited for clarity, legal issues, length and related reasons at the editor’s discretion. WHAV also reserves the right to refuse to publish submitted letters for the same reasons. All letters must be signed.